Patterns of rural infant mortality
By Paul Atkinson (University of Liverpool) – research conducted at Lancaster University thanks to ERC funding.
—
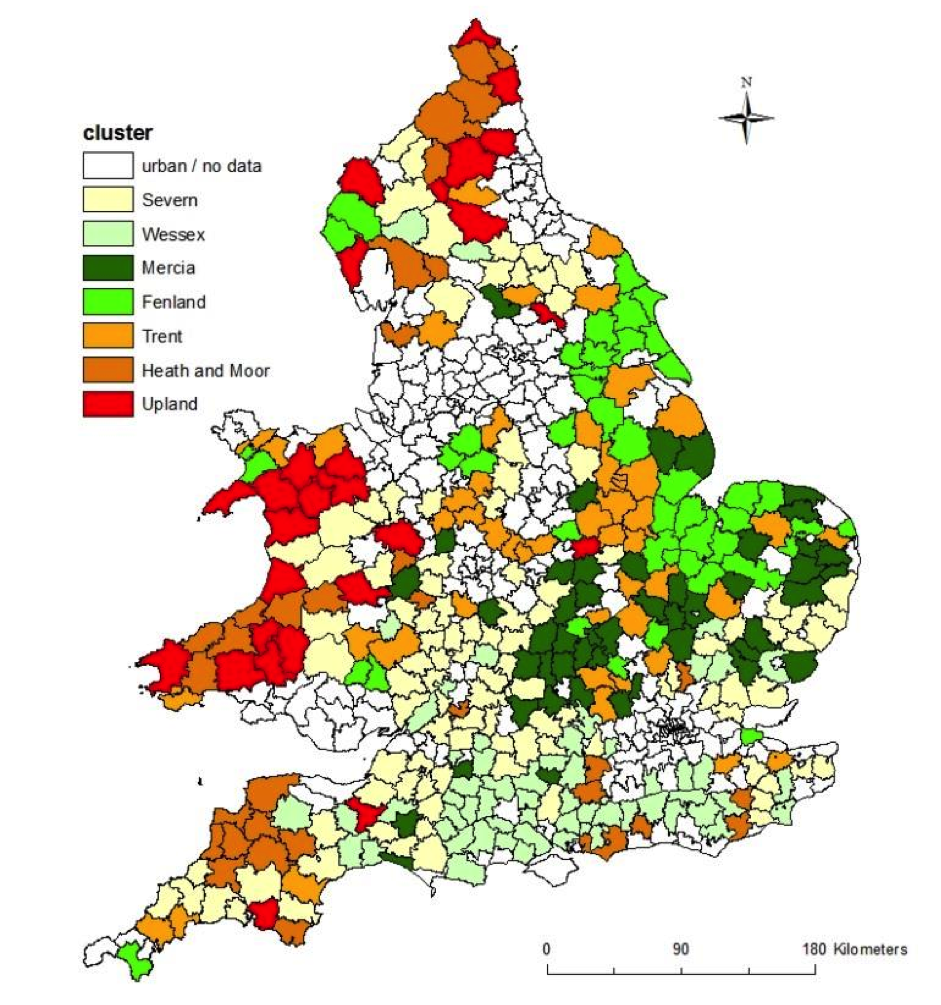
This work looked at the variation in infant mortality across time and place in country districts of England and Wales between 1851 and 1911. It used statistical methods to find patterns in the data from nearly 90% of rural places to show that, far from being one undifferentiated whole, the countryside was divided into zones with their own infant mortality trends. Broadly, infant mortality in the 1850s was worst in an eastern zone of England, but improved fastest here; across a large zone of south and central England infant mortality was somewhat lower than in the first zone in the 1850s (especially in the far south), but dropped somewhat more slowly; while in northern and western England, and in Wales, infant mortality began at lower levels than the rest of the country but stagnated or even increased, above all in the remotest districts.
How infant mortality changed in seven clusters of Registration Districts: for their locations, see map. The eastern zone is made up of Fenland and Mercia; Wessex, Severn and Trent form the south-central one and Health and Moor and Upland the final zone.

The obvious question is what made these patterns? Mainly different factors from the ones operating in towns, where the combination of crowding and poor sanitation made diarrhoeal disease the major killer, and where falling fertility was associated with decreasing infant mortality. This research identified statistically three other factors associated with infant mortality across time.
First, maternal health – plainly a factor in towns as well, but partly masked there by stronger influences. This work confirms – using a much larger dataset – Millward and Bell’s finding that the mortality of females from tuberculosis at reproductive ages, a good indicator of their general health, predicted infant mortality, explaining about a quarter of the variation in it. So, what makes mothers sick makes babies sick: probably poor nutrition above all, though we could not test that directly.
Second, maternal education, again relevant in towns too, but obscured there. Horrell, Oxley and Humphries have shown how a disadvantaged status within the household for women could produce excess female mortality: the research extends this argument to their babies. Literate women had higher status and more access to resources including food. What makes mothers vulnerable – in our study, their illiteracy – makes babies vulnerable. Female literacy predicted about a sixth of the variation in infant mortality.
The third factor linked with rising infant mortality in this period was remoteness, measured as the distance from the centre of each district to London. This was not just a characteristic of very remote locations, but applied at all distances above 100km. Exactly why infant mortality in the remotest places improved most slowly – even went backwards until the 1890s – is not very clear. This research argues that it was a mixture of large-scale out-migration stripping regions of their healthier inhabitants; possibly, the gradual way new ideas about infant care may have diffused from the biggest cities into the country, and, probably, features of rural social organisation: we argue elsewhere that the general trend to force women out of the agricultural labour market across the later nineteenth century was excluding them from forms of labour which benefited their status, and their babies’ welfare, in northern and western upland, pastoral farming areas, but harmed them in the arable south and east.
This amounts to an argument for two things: attention to ‘the mother as medium’ when explaining infant mortality rates, and attention to the diversity and particularity of local economies and cultures as we study the countryside of the past.
The full paper is available here
To contact the author: @PaulAtk43202349

